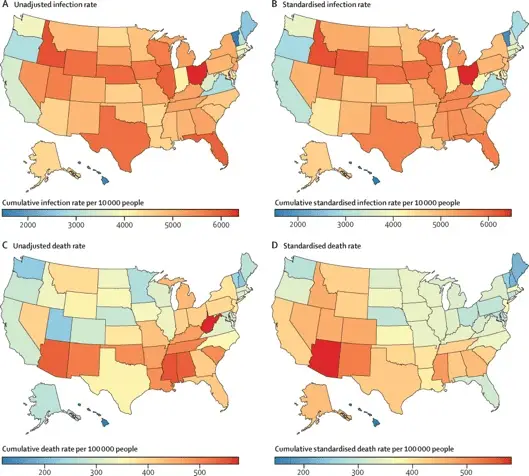
This post brings together a two topics of research into Long-Covid. Full disclosure. I do primary care for a relative suffering from Long-Covid. I live in Arizona, which according to a Lancet study, is the state with the highest adjusted death rate in the United States during the COVID-19 pandemic. Here is a link to the map.
As reported in Scientific American, “As of February 2022, the syndrome was estimated to affect about 16 million adults in the U.S. and had forced between two million and four million Americans out of the workforce, many of whom have yet to return.”
Who are these 16 million adults, their families, and the communities that sustain them? What are the long-term medical, social, and economic consequences of a disease that not everyone knows exists? Or that some people deny it existed in the first place? “Long COVID often arises in otherwise healthy young people, and it can follow even a mild initial infection. The risk appears at least slightly higher in people who were hospitalized for COVID and in older adults (who end up in the hospital more often). Women and those at socioeconomic disadvantage also face higher risk, as do people who smoke, are obese, or have any of an array of health conditions, particularly autoimmune disease. Vaccination appears to reduce the danger but does not entirely prevent long COVID.”
Several recent research studies have concluded that Long-Covid is a neurological disease affecting the brain and the nervous system. Learning from the post-viral effects of the human immunodeficiency virus (HIV) offers a roadmap on what questions to ask and how to conduct valuable research to find relief for these emerging symptoms in more and more people.
Check out recent data on the number of people who reported having Long-Covid symptoms. The numbers can only tell part of the story due to various reasons discouraging reporting.
“I now think of COVID as a neurological disease as much as I think of it as a pulmonary disease, and that’s definitely true in long COVID,” says William Pittman, a physician at UCLA Health in Los Angeles, who treats Ghormley and many similar patients.
Second, special immune cells called monocytes might be the cause of Long-Covid. This is one of the conclusions from a group of thirty-eight researchers from greater Manchester, England, published in the March 2023 issue of the European Respiratory Journal.
“Monocytes are immune cells that recognize invading pathogens and call for help from other immune cells. When they send out a signal to the rest of the immune system, other immune cells are funneled towards that signal.”
Dr. Elizabeth Mann states, “These debilitating symptoms [of Long-Covid] include extreme fatigue, shortness of breath, myalgia, brain fog, depression, fibrotic lung disease, and pulmonary vascular disease, and we now know this can last for many months or even years following infection. But treatment options for long COVID are currently limited, since the development of targeted therapeutic strategies requires an in-depth understanding of the underlying immunological pathophysiology. Our work finding a link between monocyte function and specific long COVID symptoms may provide an important first step on the road to possible treatments.”
The research collaborative concludes, “Our data define unique monocyte signatures that define subgroups of long COVID patients, indicating a key role for monocyte migration in COVID-19 pathophysiology. Targeting these pathways may provide novel therapeutic opportunities in COVID-19 patients with persistent morbidity.”
The emphatic use of the diagnosis Long-Covid is intentional; there continues to be open-ended (after) effects of the ongoing pandemic, so post-Covid seems premature – even as a medical diagnosis given the ongoing research into the impacts on the immune system. Because Covid-19 is a vascular disease that moves through the blood vessels through all other systems, the ongoing and evolving effects of health policies’ are yet to be fully revealed. Similar to how the consequences of Covid-19 continue circulating in the body after infection, misinformation continues to spread through the body politic. The medical knowledge possible about the impact of Long-Covid on people, their families, and public health is also predicated on resources for research and the political will to factor in long-term health-related issues for the ongoing pandemic. Yes, the World Health Organization declared an “end to the Covid-19 emergency,” but that does not mean the pandemic is over.
The Scientific America article quoted above is one of the most comprehensive and accessible explanations of Long-Covid, interviewing patients, their families, and researchers. Regardless of your concern level, it might be helpful to consider questions about public health and policy, social life, and the future of people living with a disease that fewer and fewer people, including some health professionals, seem worried about.









Leave a Reply